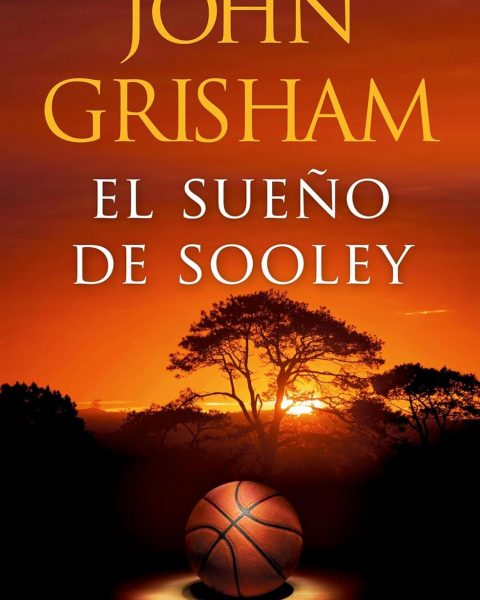
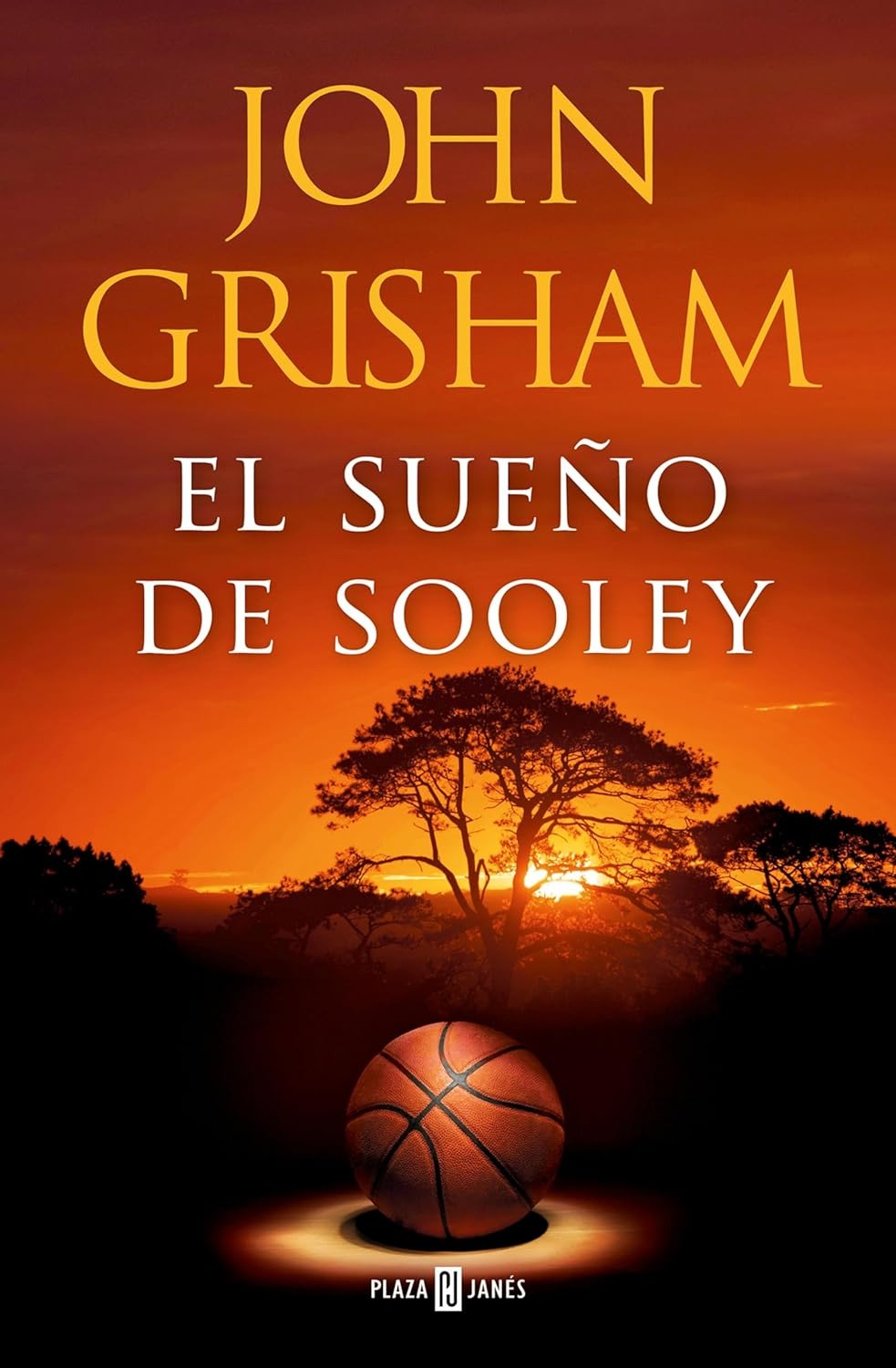
¡John Grisham Anota de Tres con “El Sueño de Sooley”! 🏀📚 Una Novela que Cambia el Juego: Descubre cómo “El Sueño de
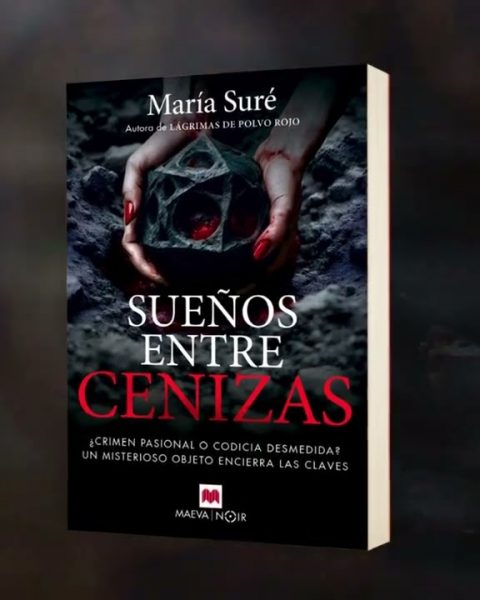
More‘Sueños entre cenizas’ de María Suré: un asesinato entre secretos arqueológicos Una novela apasionante que enfrenta a un equipo de investigadores con
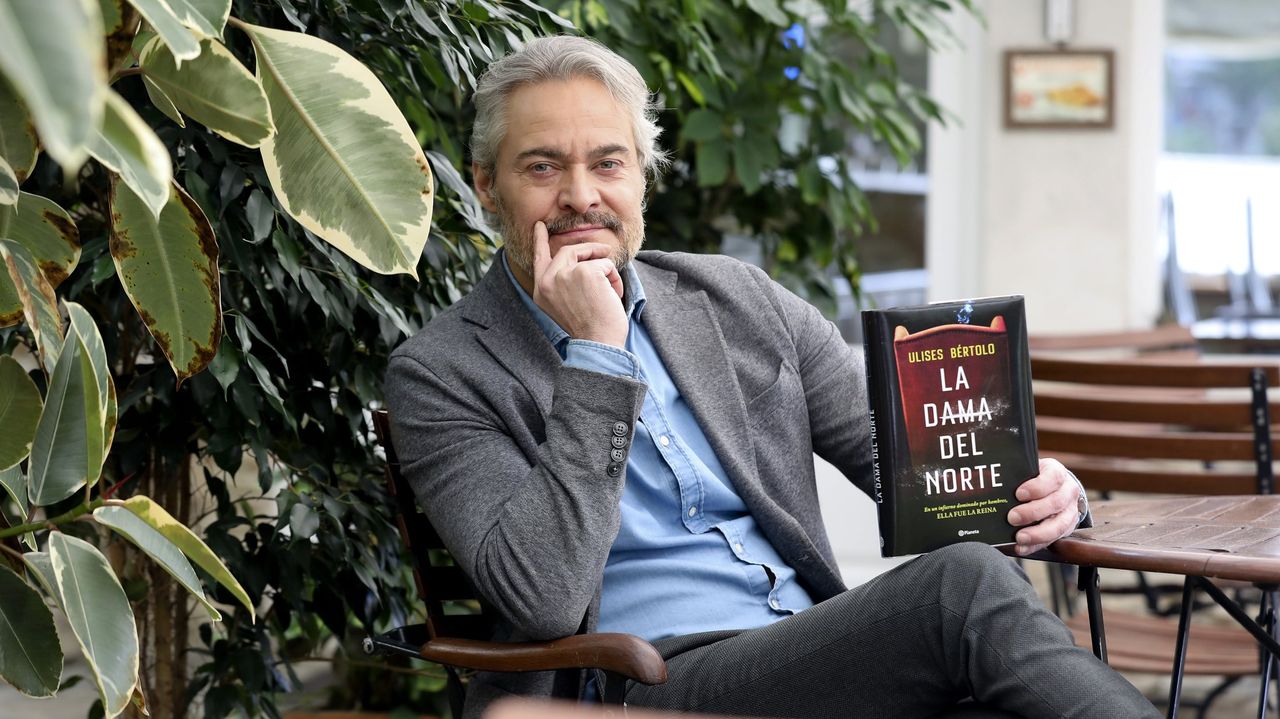
MoreLa Verdadera Historia Detrás de “La Dama del Norte”: Descubriendo a la Única Narcotraficante Líder en Galicia ¿Estás listo para desvelar el
More“El Comerciante del Cielo”: un viaje literario que une culturas y generaciones “El Comerciante del Cielo” por Estela Barrionuevo – Un puente
MoreLa Tiránica Inmoralidad del Igualitarismo: ¿Es Nuestra Obsesión con la Igualdad un Retroceso Social? 📚 ¡Descubre por qué perseguir la igualdad podría
MoreEl Viaje Redentor de Peter Kaldheim en “El Viento Idiota” Descubriendo “El Viento Idiota” – La épica transformación de Peter Kaldheim En
More¿Te atreverías a descubrir quiénes son realmente los villanos en tu vida? 📘👹 ¡El thriller literario que ha revolucionado TikTok ahora puede
More¡Explorando el Infinito! Audiolibros Futuristas que Cambiarán tu Percepción del Universo y Viajar a Otros Mundos. ¿Alguna vez te has preguntado qué
More¿Es el Melasudismo la Clave para una Vida Feliz? Descubre el Melasudismo con Pablo Álvarez ♂️ y su enfoque desenfadado para una
More¿Qué Misterios Nos Esperan en “Las Cenizas de Babilonia”, el Sexto Libro de The Expanse? ¡Explora el universo de “Las Cenizas de
MoreHijas de Raxiris: Crónicas de Raxiris 2 Ricardo Pallejá Herrera (Autor) Descargar: EUR 2,99 (Visita la lista Las últimas novedades
More¿Qué libro prohibido buscaban los personajes de “Hombres buenos” de Arturo Pérez-Reverte? Descubre “Hombres buenos” de Pérez-Reverte: Aventura Literaria en la Ilustración
More¿Cómo Transformar la Gestión Empresarial en Solo 50 Minutos? Descúbrelo con “El nuevo mánager al minuto” 🌟 Transforma tu liderazgo y eficiencia
More¿Cómo Aprender Inglés de Manera Efectiva? Guía Completa por Niveles. Los Mejores Libros y Recursos 📘✨ Te voy a aconsejar algunos de
More¿Quién es Blue Jeans, el escritor que revoluciona la literatura juvenil desde París? 📚✨ Descubre a Blue Jeans: El fenómeno español que
More¿Quién es Anna-Marie McLemore? Una voz que susurra entre lo real y lo mágico Conoce a Anna-Marie McLemore: Un viaje literario entre
More¿Cómo Convertirse en un Experto del iPhone 12 Pro sin Esfuerzo? Guía Definitiva para Principiantes 📱✨ Adentrarse en el universo del iPhone
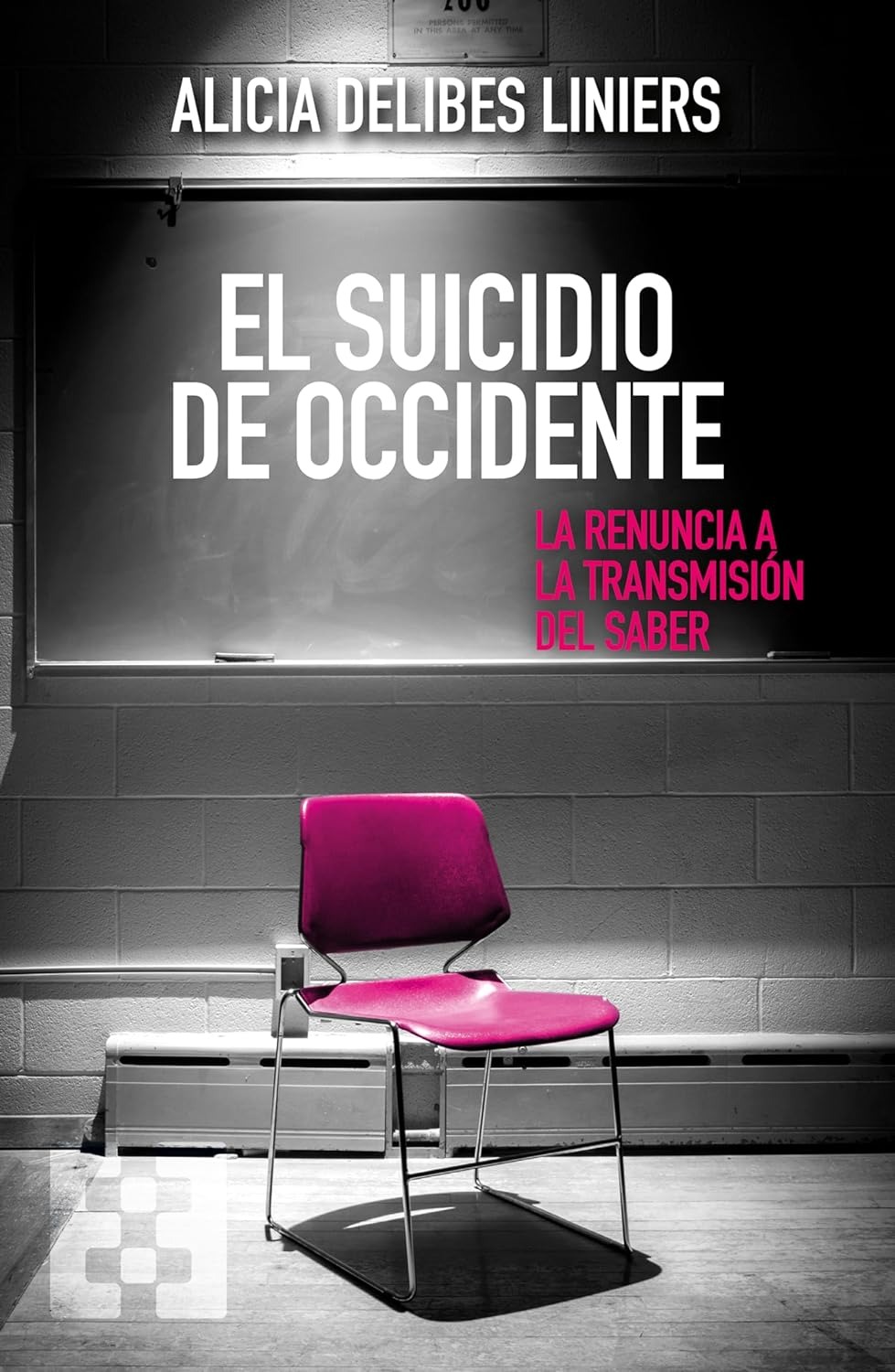
MoreEl Intrigante Declive Educativo: Desentrañando “El Suicidio de Occidente” 📚🔍 “El Suicidio de Occidente”: Análisis, Crisis Educativa y Soluciones Futuras 🌍🎓 En
MoreEl lobo de los cuentos: Cuentos infantiles de 3 a 6 años Elena Gromaz Ballesteros (Autor) (1)Fecha de publicación: 29 de noviembre
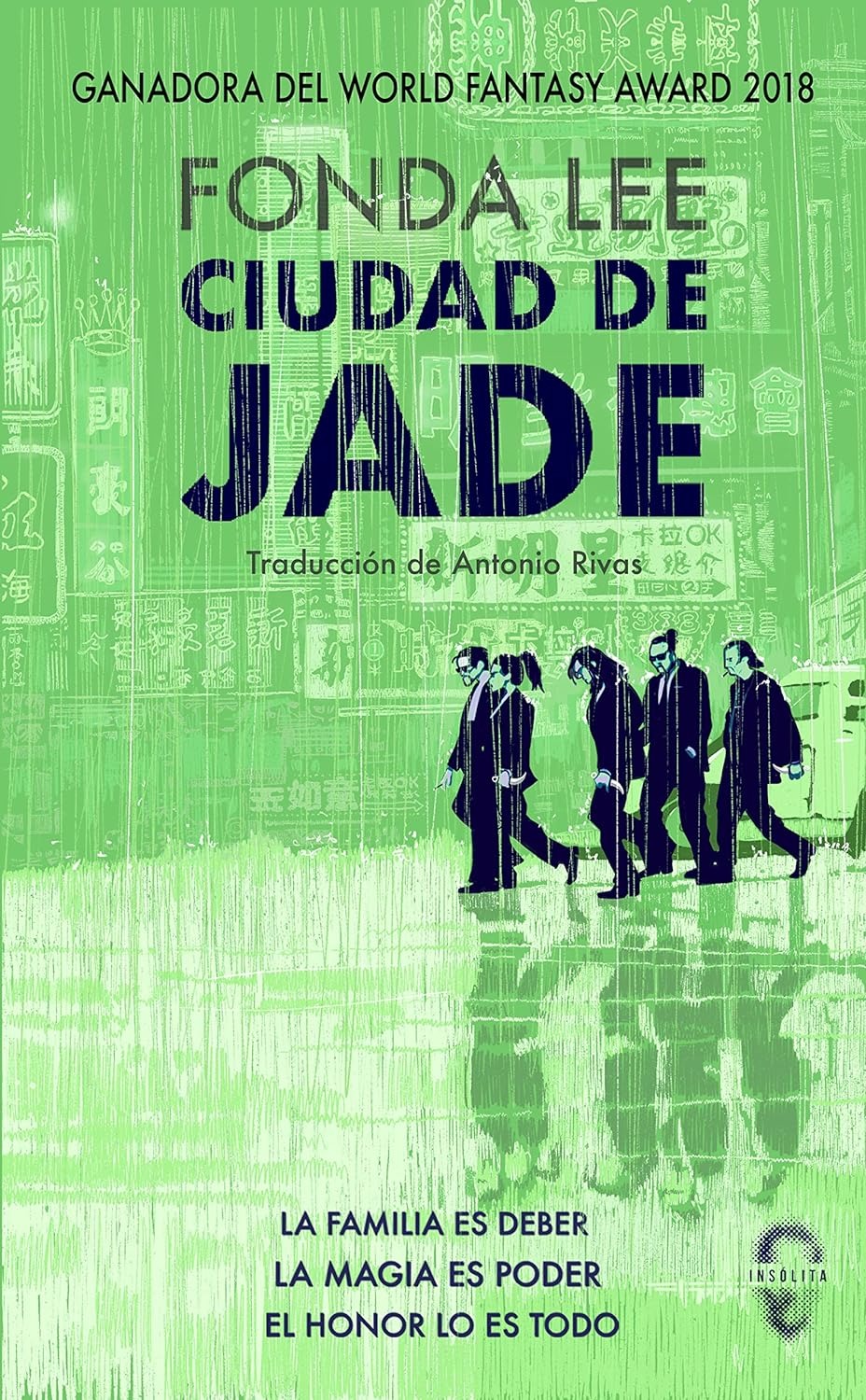
MoreMagia y Mafia bajo la Sombra del Jade: Descubriendo la Ciudad de los Secretos 🔮✨ Una Saga de Honor y Familia 🐉🏮”
MoreCésar Pérez Gellida: Maestro de la Novela Negra con Más de 300.000 Lectores. César Pérez Gellida: El Arquitecto de la Sombra en
MoreWhatsApp, Misterio y Crimen: El Enigma de “Loor” Desvelado 🔍📲💔 Un mensaje que lo cambia todo ¿Un WhatsApp puede ser el inicio
MoreSuspense y Secretos Bajo el Sol de Extremadura: Un Viaje Literario Retro con “Bajo Tierra Seca” 🔍📚 El enigma de una hacienda
MoreENTREVISTA: La Visión Profunda en “Intemperie” de Jesús Carrasco, un Análisis Futurista META TITLE: “Descifrando ‘Intemperie’: Entre Líneas con un Espía Literario”
MoreMistborn. Imperio Final - Nueva Edición (NB NOVA) Brandon Sanderson (Autor), Rafael Marín Trechera (Traductor) (49)Fecha de lanzamiento: 7 de septiembre de
MorePresencias Góticas: Un Viaje Literario Futurista al Corazón del Terror 📚✨ Explora el Futuro del Pasado con “Presencias”: Terror Gótico Renovado ✨📚
MoreLos Mejores Libros para Inspirar a tu Equipo a Alcanzar las Estrellas 🌟📚 🌟 Libros para Motivar Equipos 📚✨ En el universo
More